Human Papillomavirus (HPV) DNA Detector
For cervical cancer prevention, the Human Papillomavirus (HPV) DNA Detector Test emerges as a pivotal diagnostic tool. Understanding its significance & functionality is crucial in comprehending its role as a cervical cancer marker. Read this blog to know that what the HPV DNA Detector Test entails, why it is important, and how it contributes to the early detection of cervical cancer.Book an HPV DNA Detector Test in Bhadreswar for ONLY ₹1450*
What Is The HPV DNA Detector Test?
Human Papillomavirus (HPV) DNA Detector Test Price in Bhadreswar - Compare Prices at 2 Labs
Name
Proc. Time
Rating
Price
Health Conditions That Can Be Detected Through An HPV DNA Detector Test
The Human Papillomavirus (HPV) DNA Detector, primarily utilised as a cervical cancer marker, can also aid in detecting several other health conditions related to HPV infections. Here are some notable conditions that can be identified through this diagnostic tool:
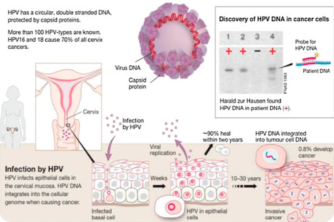
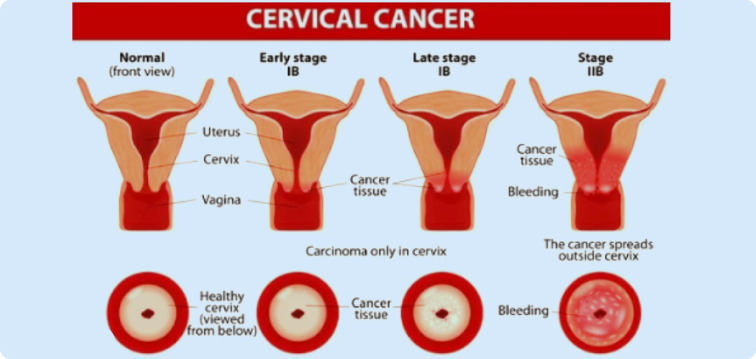
Cervical Cancer: The primary purpose of the HPV DNA Detector is to screen for cervical cancer. Persistent infection with high-risk HPV strains is a significant risk factor for the development of cervical cancer. By detecting HPV DNA in cervical cells, the test can identify women at risk of developing or already having cervical cancer.
Pre-cancerous Cervical Lesions: HPV infections can lead to the development of pre-cancerous lesions in the cervix, known as cervical dysplasia or cervical intraepithelial neoplasia (CIN). These lesions, if left untreated, can progress to cervical cancer. The HPV DNA Detector can detect HPV DNA in cervical cells, indicating the presence of pre-cancerous changes and enabling early intervention to prevent the progression to cancer.
Genital Warts: Certain strains of HPV can cause genital warts, which are benign growths on the genital and anal areas. While not cancerous, genital warts can cause discomfort and affect a person's quality of life. The HPV DNA Detector may detect HPV DNA associated with wart-causing strains, aiding in the diagnosis and management of genital warts.
Oropharyngeal Cancer: HPV infection has been implicated in the development of oropharyngeal (throat) cancer. HPV-related oropharyngeal cancer has become increasingly prevalent in recent years. While the HPV DNA Detector is primarily used for cervical cancer screening, it may also have potential applications in detecting HPV-related cancers in other anatomical sites, including the oropharynx.
Anal Cancer: HPV infection is a significant risk factor for anal cancer, particularly among individuals with a history of anal intercourse or immunocompromised individuals. The HPV DNA Detector may be used to detect HPV DNA in anal cells, aiding in the early detection and management of anal cancer.
Who Should Get Tested?
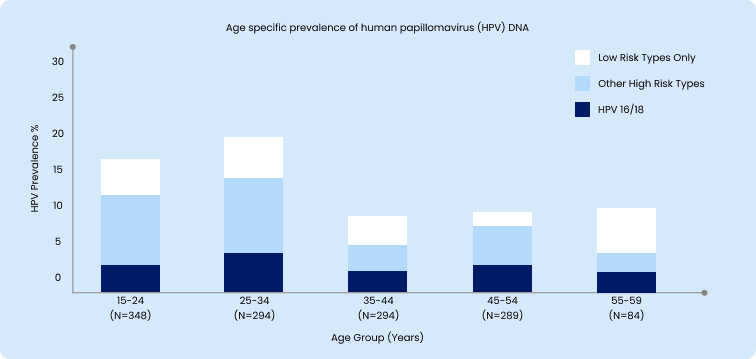
Determining who should undergo testing with the Human Papillomavirus (HPV) DNA Detector depends on several factors. Primarily, routine cervical cancer screening, including HPV DNA testing, is recommended for women starting at age 21. This screening is vital as cervical cancer typically develops slowly, often starting with pre-cancerous changes that may not exhibit noticeable symptoms in the early stages. Additionally, individuals with abnormal Pap smear results or experiencing symptoms associated with HPV infection, such as genital warts or abnormal vaginal bleeding, should consider HPV DNA testing. Moreover, those engaging in high-risk sexual behavior, such as having multiple sexual partners or engaging in unprotected sex, are at increased risk and may benefit from HPV testing as part of comprehensive sexual health screening. Immunocompromised individuals and individuals with a history of HPV-related conditions should also undergo regular HPV DNA testing for surveillance and early detection of HPV infections and associated complications. Overall, consultation with a healthcare provider is essential to determine the most appropriate testing strategy based on individual risk factors and medical history..Book an HPV DNA Detector Test in Bhadreswar for ONLY ₹1450*
| Current cervical cancer screening recommendations | |
|---|---|
| Age 20 or younger | No screening required |
| 21-29 | Pap test every 3 years; no HPV screening |
| 30-65 | Pap test every 3 years, or a pap test and HPV test together every 5 years |
| 66 or older | No more screening needed if you’ve had 3 normal pap tests or 2 normal HPV tests in a row |
How Is The Testing Done?
STEP 1.Sample Collection:The first step in HPV DNA testing is the collection of cervical cell samples. This is often done during a pelvic exam using a device called a speculum to visualize the cervix. A healthcare provider uses a swab or brush to gently collect cells from the surface of the cervix. In some cases, samples may also be collected during a Pap smear or HPV test.
STEP 2.Sample Processing:Once collected, the cervical cell samples are processed in the laboratory to prepare them for analysis. This may involve separating the cells from any mucus or debris and extracting the DNA from the cells.
STEP 3.HPV DNA Detection:The extracted DNA is then subjected to molecular testing techniques to detect the presence of HPV DNA. Polymerase chain reaction (PCR) is the most common method used for HPV DNA detection. PCR amplifies specific regions of the HPV DNA, making it easier to identify and analyze.
STEP 4.HPV Typing:After HPV DNA detection, further analysis may be performed to determine the specific HPV types present in the sample. This is important because not all HPV strains pose the same risk for cervical cancer. High-risk HPV strains, such as HPV types 16 and 18, are more strongly associated with cervical cancer development.
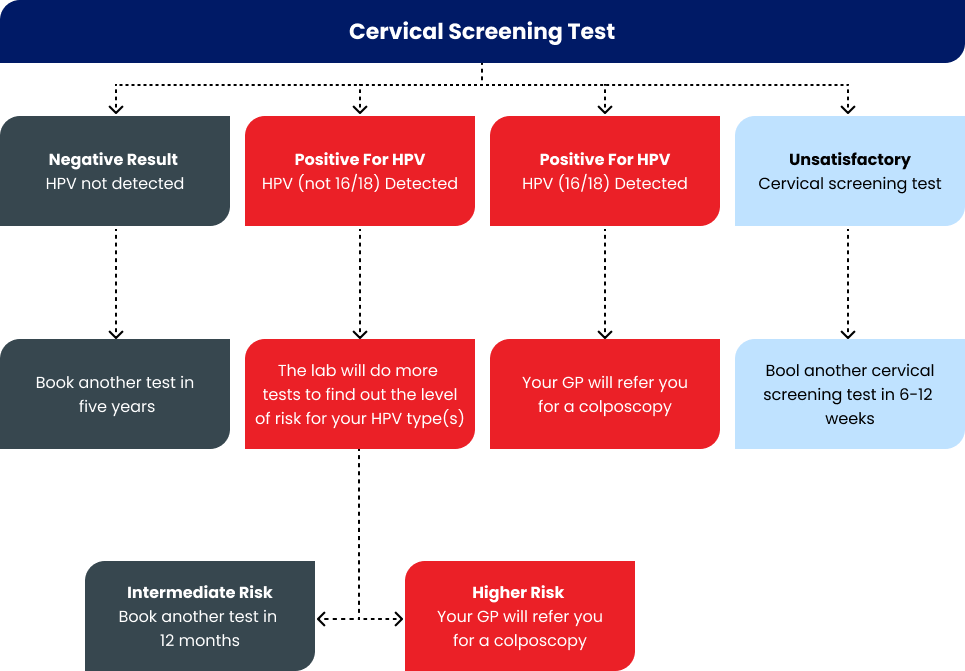
STEP 5.Result Interpretation:Once the testing is complete, the results are interpreted by healthcare professionals. A positive result indicates the presence of HPV DNA in the cervical cells, while a negative result indicates the absence of detectable HPV DNA. In cases of a positive result, the specific HPV types detected and their risk level (high-risk or low-risk) may also be reported.
STEP 6.Follow-Up and Management:Depending on the test results and individual circumstances, follow-up procedures may be recommended. This may include additional testing, such as colposcopy or biopsy, to evaluate any abnormal cervical findings and determine the need for further treatment or surveillance.
How To Prepare For The Test?
Schedule The Test: Contact your healthcare provider to schedule the HPV DNA Detector Test. You may need to schedule the test at a specific time in your menstrual cycle, depending on the provider's recommendations.
Avoid Vaginal Products: In the days leading up to the test, avoid using vaginal products such as tampons, vaginal creams, foams, or douches. These products can interfere with the test results by contaminating the cervical cell samples.
Timing Considerations: If you are menstruating, you may need to reschedule the test for a time when you are not actively bleeding. Menstrual blood can also interfere with the test results.
Inform Your Healthcare Provider: Inform your healthcare provider about any medications you are taking, especially if you are using hormone-based contraceptives or medications that may affect your menstrual cycle. Your healthcare provider may need to consider these factors when interpreting the test results.
Comfort Measures: If you are anxious or uncomfortable about the test, consider discussing your concerns with your healthcare provider beforehand. They can provide reassurance and answer any questions you may have about the procedure.
Follow Pre-Test Instructions: Your healthcare provider may provide specific pre-test instructions based on your individual circumstances. Follow these instructions carefully to ensure accurate test results.
Relaxation Techniques: If you experience discomfort or anxiety during the test, practice relaxation techniques such as deep breathing or visualization to help you stay calm and comfortable.
What Does The Test Results Mean?
A "normal" or negative result from the HPV DNA test suggests that the individual tested does not have an active high-risk HPV infection in the cervix. However, it's important to note that a negative result does not necessarily mean complete immunity to HPV or protection against future infections. Additionally, it does not rule out the possibility of previous exposure to HPV or the presence of low-risk HPV strains that may not be detected by the test. The normal range for the HPV DNA test provides reassurance regarding the absence of high-risk HPV infection at the time of testing. It indicates a lower risk of developing cervical cancer or pre-cancerous lesions associated with high-risk HPV strains. However, regular cervical cancer screening, including HPV testing, is still recommended according to guidelines provided by healthcare professionals to monitor for any changes in HPV status over time..
| Pap Result | Disease Category* | |||||
|---|---|---|---|---|---|---|
| Normal | Abnormal | Abnormal Med & High | ||||
| HPV DNA | HPV DNA | HPV DNA | ||||
| Positive | Negative | Positive | Negative | Positive | Negative | |
| LSIL | 14 | 8 | 84 | 24 | 51 | 9 |
| ASCUS | 20 | 19 | 30 | 21 | 17 | 3 |
| Normal | 59 | 147 | 58 | 97 | 30 | 11 |
| Total | 98 | 176 | 185 | 144 | 254 | 30 |

Risks Associated With The Test
Discomfort or Pain: During the test, some individuals may experience mild discomfort or pain when the cervical cell sample is collected using a swab or brush. However, discomfort is usually brief and minimal.
False-Positive Results: Like any diagnostic test, the HPV DNA test is not perfect and may produce false-positive results, indicating the presence of high-risk HPV when it is not actually present. False-positive results can lead to unnecessary anxiety and follow-up testing, such as colposcopy or biopsy, which may carry additional risks.
False-Negative Results: Similarly, false-negative results can occur, indicating the absence of high-risk HPV when it is actually present. False-negative results may provide a false sense of security and delay further evaluation and treatment, potentially allowing cervical abnormalities to progress unnoticed.
Psychological Impact: Receiving positive or abnormal HPV DNA test results can cause emotional distress, anxiety, or fear of developing cervical cancer. It's important for individuals to receive appropriate counseling to address psychological or emotional concerns related to HPV testing and cervical cancer screening.
Overdiagnosis and Overtreatment: Detecting low-risk HPV infections or minor cervical abnormalities through HPV DNA testing may lead to overdiagnosis and overtreatment of conditions that would not have progressed to cervical cancer or cause harm. This can result in unnecessary medical interventions, such as colposcopy, biopsy, or treatment procedures, which carry their own risks and potential side effects.
Lifestyle Tips To Maintain Cervical Health
Practice Safe Sex:
Use condoms consistently and correctly during sexual activity to reduce the risk of HPV and other sexually transmitted infections (STIs).
Limit the number of sexual partners to reduce the risk of exposure to HPV and other STIs.
Get Vaccinated:
Vaccination against HPV is a highly effective way to prevent infection with high-risk HPV strains that can lead to cervical cancer and other HPV-related cancers.
The HPV vaccine is recommended for both males and females, ideally before becoming sexually active. Speak to your healthcare provider about HPV vaccination options.
Don't Smoke:
Smoking has been linked to an increased risk of cervical cancer and other HPV-related conditions.
Quit smoking or avoid exposure to secondhand smoke to reduce your risk of cervical cancer and promote overall health.
Maintain a Healthy Diet:
Eat a balanced diet rich in fruits, vegetables, whole grains, and lean proteins.
Aim to maintain a healthy weight, as obesity is associated with an increased risk of cervical cancer.
Exercise Regularly:
Engage in regular physical activity to support overall health and maintain a healthy weight.
Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity per week, as recommended by health guidelines.
Practice Good Hygiene:
Maintain good genital hygiene to reduce the risk of genital infections, including HPV.
Avoid using harsh or irritating products in the genital area, such as douches or scented feminine hygiene products.
Attend Regular Check-ups:
Schedule regular gynecological check-ups and cervical cancer screenings according to guidelines provided by your healthcare provider.
Stay informed about the recommended screening intervals for Pap smears, HPV testing, and other cervical cancer screening tests based on your age and individual risk factors.
Manage Stress:
Practice stress-reduction techniques such as mindfulness, meditation, yoga, or deep breathing exercises to manage stress levels and promote overall well-being.
*T&Cs Apply