About The Knee Joint
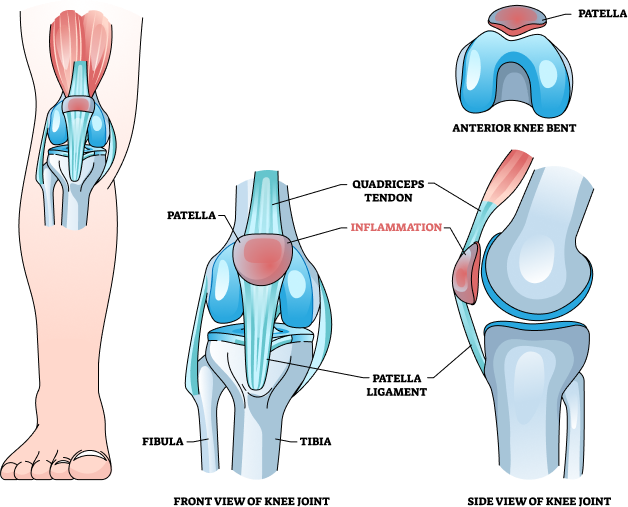
The knee joint is a complex hinge joint that connects the thigh bone (femur) to the shin bone (tibia). It also involves the smaller bone located next to the tibia, known as the fibula, and the kneecap (patella). The knee joint is one of the largest and most important joints in the body, essential for movement and bearing the body weight. The knee joint is one of the most complex and vital joints in the human body, enabling a wide range of movements and bearing significant loads. Lets understand the structure of the knee.
| Structure | Components |
|---|---|
| Bones | Femur (Thigh Bone) |
| - | Tibia (Shin Bone) |
| -- | Fibula |
| --- | Patella (Kneecap) |
| Cartilage | Articular Cartilage |
| Menisci (Medial Meniscus, Lateral Meniscus) | |
| Ligaments | Anterior Cruciate Ligament (ACL) |
| . | Posterior Cruciate Ligament (PCL) |
| .. | Medial Collateral Ligament (MCL) |
| ... | Lateral Collateral Ligament (LCL) |
| Muscles | Quadriceps |
| ,,,, | Hamstrings |
| Nerves | Femoral Nerve |
| , | Sciatic Nerve |
| ,, | Tibial Nerve |
| ,,, | Common Peroneal Nerve |
MRI KNEE Available In
Name
Proc. Time
Rating
Price
What Is An MRI Of Both Knee Joints?
MRI Both Knees refers to a medical imaging procedure in which Magnetic Resonance Imaging (MRI) is performed on both knee joints simultaneously. This diagnostic technique allows for the generation of detailed images of the internal structures, including bones, cartilage, ligaments, tendons, and surrounding soft tissues, in both knees. By imaging both knees, healthcare professionals can assess for symmetry, identify bilateral abnormalities, and provide comprehensive diagnosis of knee-related conditions. BOOK AN MRI KNEE FOR ₹7000*
Purpose Of Both Knee Joints MRI?
The purpose of an MRI of both knee joints is to provide a detailed and comprehensive evaluation of the internal structures within both knees. This advanced imaging technique is essential for accurately diagnosing a wide range of knee-related conditions, including ligament and meniscal tears, cartilage damage, and tendon injuries. Additionally, it is invaluable for identifying degenerative diseases such as osteoarthritis and rheumatoid arthritis, as well as detecting inflammation, tumours, and cysts. By capturing high-resolution images of both knees, MRI allows healthcare professionals to compare the joints, assess symmetry, and detect bilateral abnormalities. This is particularly useful for athletes, individuals with chronic knee pain, and patients with conditions that may affect both knees. Furthermore, MRI is instrumental in evaluating the effectiveness of surgical interventions, such as knee arthroscopy or knee replacement, by providing clear post-operative images. Overall, an MRI of both knee joints is a critical diagnostic tool that enhances the ability of medical professionals to develop accurate treatment plans and monitor the progress of knee-related conditions.
Which Health Conditions Can Be Diagnosed?
An MRI of both knee joints is a valuable diagnostic tool for detecting a wide range of health conditions and injuries. Some of the health conditions diagnosed by MRI of both knee joints include:
Ligament Injuries: ACL (anterior cruciate ligament) tears, PCL (posterior cruciate ligament) tears, MCL (medial collateral ligament) tears, and LCL (lateral collateral ligament) tears.
Meniscal Tears: Tears or injuries to the menisci (medial and lateral), which are C-shaped cartilage structures that act as shock absorbers in the knee joint.
Cartilage Damage: Articular cartilage injuries or defects, such as osteochondral lesions or chondral defects, which can lead to joint pain and osteoarthritis.
Tendon Injuries: Tears or inflammation of tendons around the knee, including the patellar tendon, quadriceps tendon, and hamstring tendons.
Osteoarthritis: Degenerative joint disease characterized by the breakdown of cartilage and the formation of bone spurs, resulting in joint pain, stiffness, and reduced mobility.
Rheumatoid Arthritis: An autoimmune disorder causing inflammation of the synovial membrane lining the joints, leading to pain, swelling, and joint deformity.
Bursitis: Inflammation of the bursae, small fluid-filled sacs that cushion the knee joint, resulting in pain and swelling around the knee.
Bone Fractures: Fractures or stress fractures of the femur, tibia, patella, or other bones within or around the knee joint.
Synovial Disorders: Conditions affecting the synovial membrane, such as synovitis or pigmented villonodular synovitis (PVNS), leading to joint inflammation and pain.
Tumours And Cysts: Benign or malignant tumours, cysts, or other abnormal growths within or around the knee joint, which may require further evaluation and treatment.
By providing detailed images of the internal structures of both knee joints, MRI helps healthcare professionals accurately diagnose these conditions and injuries, guiding appropriate treatment plans and interventions for patients.BOOK AN MRI KNEE FOR ₹7000*
Who Should Get Tested?
An MRI of both knee joints is recommended for a variety of individuals, especially those experiencing specific symptoms or having risk factors. Here are the key groups of people who should consider getting an MRI:
Athletes & Active Individuals: Athletes and active individuals participating in high-impact sports or activities that stress the knees, such as running, basketball, soccer, and skiing, may benefit from an MRI to diagnose potential knee injuries like ligament tears and meniscal damage.
Individuals With Persistent Knee Pain: People experiencing chronic knee pain that does not respond to initial treatments or physical therapy should consider getting an MRI to identify underlying issues such as cartilage damage, degenerative conditions, or other structural abnormalities.
Individuals With Acute Knee Injuries: Anyone who has sustained a knee injury from a fall, collision, or other trauma should get an MRI to assess for fractures, ligament tears, or tendon injuries to ensure appropriate treatment and recovery plans.
Patients With Inflammatory Joint Diseases: Individuals diagnosed with conditions like rheumatoid arthritis or other autoimmune disorders may need an MRI to evaluate the extent of joint inflammation, synovitis, and damage to the knee structures.
Older Adults With Osteoarthritis Symptoms: Older adults experiencing symptoms like joint stiffness, swelling, and reduced mobility can benefit from an MRI to assess the severity of cartilage degradation and bone changes.
Individuals Undergoing Pre-Surgical Planning & Post-Surgical Assessment: Individuals preparing for knee surgery, such as ligament reconstruction or meniscal repair, and those undergoing post-operative evaluation may require an MRI to plan the procedure or assess the success of the surgery and healing process.
Individuals With Unexplained Knee Symptoms: Anyone experiencing unexplained knee symptoms such as swelling, instability, locking, or decreased range of motion should consider an MRI to diagnose potential underlying conditions like cysts or tumours.
Individuals With Suspected Knee Tumours: People showing signs of a tumour or cyst in the knee, such as localised pain, swelling, or a palpable mass, should get an MRI for detailed evaluation and diagnostic treatment.
Patients With Previous Knee Surgery: Individuals who have undergone knee surgeries and are experiencing new or recurring symptoms should consider an MRI to check for complications that may have arisen post-surgery.
By identifying the specific conditions and providing a detailed view of the knee’s internal structures, an MRI of both knee joints can help healthcare professionals develop accurate diagnoses and effective treatment plans for these individuals BOOK AN MRI KNEE FOR ₹7000*
| MRI Scans | City | Price | ||
|---|---|---|---|---|
| 1 | MRI Knee Both Joints | - | 7000 |
How The Scan Is Done?
Preparation
Patient Screening: Before the scan, patients undergo screening to ensure they don’t have any contraindications, such as metal implants or pacemakers, which could interfere with the MRI machine.
Clothing and Accessories: Patients change into a hospital gown and remove metal objects like jewellery to avoid interference with the magnetic field.
Contrast Agents: Depending on the case, a contrast agent might be administered intravenously to enhance image clarity, with precautions taken for any potential allergic reactions.
During the Scan
Positioning: Patients lie on the MRI table, often with legs extended, while a specialised knee coil is positioned around the knees for focused imaging.
Remaining Still: It’s vital for patients to remain motionless during the scan to prevent blurring of images. Technologists may use cushions or straps to help patients maintain the correct position.
Communication: Patients are provided with a call button to communicate with the technologist during the scan, ensuring comfort and safety.
Image Acquisition: Multiple sets of images are taken from various angles during the 30 to 60-minute scan, with occasional brief breath-holding to minimise motion artefacts.
After the Scan:
Post-Scan Procedure: After the scan, patients are assisted off the table. If contrast was used, they’re monitored briefly for potential reactions.
Review and Results: The obtained images are reviewed by a radiologist, who interprets the findings and generates a report for the referring physician, who then prepares any necessary treatment plans.
How To Interpret The Results?
NORMAL
Intact Structures: The MRI images show the bones, cartilage, ligaments, tendons, and other soft tissues within both knee joints are intact and exhibit normal anatomy without any signs of damage, tears, or degeneration.
No Signs of Inflammation: There are no signs of inflammation or swelling in the synovial lining, bursae, or surrounding tissues, suggesting that the knees are not affected by conditions such as arthritis or bursitis.
Absence of Abnormal Growth: There are no abnormal growths, cysts, tumours, or masses detected within or around the knee joints, indicating no significant structural abnormalities or neoplastic conditions are present.
Normal Alignment: The alignment of the bones and joint spaces within both knees appears normal, indicating proper biomechanics and function of the knee joints.
No Evidence of Fluid Accumulation: There is no excessive accumulation of fluid within the joint space or surrounding tissues, which could indicate acute injury, inflammation, or infection.
Healthy Cartilage: The articular cartilage covering the ends of the bones within the knee joints appears smooth, even, and without any evidence of defects, fissures, or degeneration.
ABNORMAL
Bone Abnormalities: Abnormalities like fractures, bone marrow oedema, or osteonecrosis indicate structural damage. Fractures show as disruptions in bone continuity, while bone marrow oedema appears as increased signal, indicating inflammation or bruising. Osteonecrosis suggests dead bone tissue due to poor blood supply.
Cartilage Abnormalities: Abnormal cartilage findings, such as thinning or defects, point to degenerative conditions like osteoarthritis, leading to joint pain and reduced function. Chondromalacia patellae indicates cartilage softening under the kneecap, causing pain.
Meniscal Tears: Meniscal tears appear as irregularities in the meniscus and cause pain, swelling, and instability. Degenerative changes within the meniscus indicate chronic wear and tear.
Ligament Abnormalities: Ligament issues like tears or sprains appear as disruptions which lead to knee instability and functional impairment. Chronic changes suggest previous injuries or ongoing degeneration.
Tendon Abnormalities: Tendon problems, such as tendinopathy or tears, show up as thickened tendons or discontinuities. Tendinopathy indicates chronic irritation, while tendon tears impair knee function.
Synovial and Bursal Abnormalities: Abnormal findings in the synovial lining or bursae suggest inflammation or infection. Synovitis is linked to inflammatory conditions, and bursitis indicates repetitive stress or direct injury.
Fluid Accumulation: Excess fluid in the knee joint, known as joint effusion, is a sign of underlying issues such as inflammation, infection, or trauma. This fluid buildup indicates the knee’s response to stress or injury. Cysts like Baker’s cysts indicate chronic joint issues.
Additional Findings: Loose bodies, small fragments of bone or cartilage, cause pain and mechanical symptoms. Tumours, benign or malignant, appear as abnormal masses requiring further evaluation.
Associated Risks
Claustrophobia: Some patients may feel anxiety or claustrophobia due to the enclosed MRI machine. Open MRI machines, sedation, or relaxation techniques can help alleviate this discomfort.
Contrast Reactions: Using a contrast agent enhances imaging but poses a small risk of allergic reactions, typically mild (itching, rash), though severe reactions are rare.
Discomfort from Staying Still: Patients must remain still during the scan, which can be uncomfortable, especially for those with joint pain or stiffness.
Noise: MRI machines produce loud noises during the scanning process. Ear protection is provided, but the noise can still be bothersome for some patients.
Metal Implants and Devices: Patients with metal implants, like pacemakers or prostheses, may face risks as the MRI’s magnetic field can interfere with these devices. Informing the radiologist about this is crucial.
Pregnancy: MRI is generally avoided during the first trimester as the effects on unborn babies are not fully understood. Pregnant women should consult their healthcare provider before undergoing an MRI.
High Costs: MRI scans can be expensive, and not all insurance plans cover the cost. Checking with the insurance provider about coverage and out-of-pocket expenses is essential.
Delayed Diagnosis: Interpreting MRI results can be complex, possibly leading to delays in diagnosis or the need for further testing.
Radiation: MRI does not use ionising radiation, making it safer compared to X-rays or CT scans. Patients should discuss the necessity and frequency of imaging with their healthcare provider.
TIPS TO KEEP YOUR KNEES HEALTHY
Stay Active: Regular exercise strengthens the muscles around the knee, improving joint stability. Focus on low-impact activities like swimming, cycling, and walking to avoid unnecessary stress on the knees.
Maintain a Healthy Weight: Excess weight puts additional strain on the knees. Maintaining a healthy weight reduces the risk of developing conditions like osteoarthritis and decreases the load on your knee joints.
Strengthen Muscles: Engage in exercises that build the muscles around your knees, particularly the quadriceps and hamstrings. Include leg lifts, squats, and lunges in your workout routine.
Stretch Regularly: Incorporate stretching exercises to maintain flexibility and range of motion in the knees. Stretching the muscles around the knee can prevent stiffness and injuries.
Wear Proper Footwear: Choose shoes that provide good support and cushioning to reduce the impact on your knees. Avoid high heels and opt for shoes with a low heel and firm arch support.
Use Knee Protection: If you engage in activities that put stress on your knees, like gardening or certain sports, use knee pads or braces to provide extra support and protection.
Avoid Overexertion: Listen to your body and avoid overloading your knees with excessive activity or heavy lifting. Gradually increase the intensity of your workouts to prevent strain.
Practice Good Posture: Maintain proper posture while standing, walking, and sitting to distribute your weight evenly and reduce stress on your knees.
Keep Moving: Avoid sitting or standing in the same position for long periods. Take breaks to move around and stretch to keep your joints flexible and reduce stiffness.
Stay Hydrated: Drink plenty of water to keep your joints lubricated. Hydration is essential for maintaining healthy cartilage and reducing the risk of joint pain.
Eat a Balanced Diet: Consume a diet rich in nutrients that support joint health, such as omega-3 fatty acids, antioxidants, and vitamins. Foods like fish, nuts, leafy greens, and fruits are beneficial for joint health.
Avoid High-Impact Activities: Limit activities that involve heavy impact on the knees, such as running on hard surfaces or jumping. Opt for gentler alternatives like swimming or cycling to protect your knees.