What Is Testosterone Total?
Testosterone is a hormone primarily produced in the testicles in men and in smaller amounts in the ovaries and adrenal glands in women. It belongs to a class of hormones called androgens and is crucial for the development of male reproductive tissues and the maintenance of secondary sexual characteristics. In men, testosterone levels typically peak during adolescence and early adulthood and then gradually decline with age.
Typical Total Testosterone Levels In Children And Adolescents
| Age | Male (in ng/dl) | Female (in ng/dl) |
|---|---|---|
| 7-10 Years Old | 1.80 to 5.68 | 2.69 to 10.29 |
| 13-17 Years Old | 208.08 to 496.58 | 16.72 to 31.55 |
Testosterone Test Price in Sasara - Compare Prices at 1 Labs
Name
Proc. Time
Rating
Price
Typical Total Testosterone Levels In Adults
| Age | Male (in ng/dl) | Female (in ng/dl) |
|---|---|---|
| 19 Years and Older | 265 to 923 | 15 to 70 |
Understanding The Testosterone Total Test
The Testosterone Total Test is a simple blood test that measures the total amount of testosterone circulating in the bloodstream. It provides valuable insights into a person's overall testosterone production and can help diagnose various medical conditions related to testosterone levels. The Testosterone Total Test may be referred to by other names, depending on the context or specific aspects being measured. Some alternative names for the Testosterone Total Test include:
Purposes Of The Testosterone Total Test
Testosterone Total Levels:The test quantifies the overall concentration of testosterone in the blood, including both bound and free testosterone. Bound testosterone is attached to proteins such as albumin and sex hormone-binding globulin (SHBG), while free testosterone is not bound and is considered the biologically active form.
Testosterone Total Levels:By measuring total testosterone levels, healthcare providers can assess various aspects of hormonal health and diagnose conditions related to testosterone levels, such as hypogonadism (low testosterone) or hypergonadism (high testosterone).
Hormone Imbalances:Deviations from normal testosterone levels can indicate hormonal imbalances, which may contribute to symptoms such as fatigue, changes in libido, erectile dysfunction, infertility, mood disturbances, and changes in body composition (such as decreased muscle mass or increased fat).
Monitoring Hormone Replacement Therapy (HRT):For individuals undergoing testosterone replacement therapy (TRT) to address low testosterone levels, the Testosterone Total Test is used to monitor treatment efficacy and adjust therapy dosages as needed to achieve optimal testosterone levels and alleviate symptoms.
Assessment of Reproductive Health:Testosterone plays a crucial role in reproductive health, influencing sperm production and fertility in men. Abnormal total testosterone levels may indicate underlying factors contributing to infertility or reproductive dysfunction.
Risk Assessment for Health Conditions:Abnormal testosterone levels have been associated with various health conditions, including cardiovascular disease, metabolic syndrome, osteoporosis, and mood disorders. Monitoring total testosterone levels can help identify individuals at increased risk for these conditions and guide preventive interventions.
The recommended frequency of testosterone total testing varies depending on individual circumstances and medical needs. Typically, for men undergoing testosterone replacement therapy or monitoring testosterone levels due to certain medical conditions such as hypogonadism, the frequency of testing may be more frequent, initially every few months, and then less often once levels stabilize. For individuals with stable testosterone levels and no underlying health concerns, testing may be performed less.
| not displayed | Male Normal Reference Range | Optimal Range |
|---|---|---|
| Total Testosterone | 250-1100 ng/dL | 1000-1200 ng/dL |
| Free Testosterone | 35-155 pg/mL | 200-250 pg/mL |
| Estradiol | <39 pg/mL | 21.8-30.11 pg/mL |
| not displayed | Male Normal Reference Range | Optimal Range |
|---|---|---|
| Testosterone | 250-1100 ng/dL | 150-250 ng/dL |
| Estradiol | 35-155 pg/mL | - |
| FSH | <39 pg/mL | - |
| Progesterone | <2.7-31.4 ng/mL | - |
What Health Conditions Can Be Detected In A Testosterone Total Test?
Hypogonadism: Low testosterone levels, known as hypogonadism, can result from dysfunction in the testes or hypothalamus-pituitary-gonadal axis. Symptoms of hypogonadism may include fatigue, reduced libido, erectile dysfunction, infertility, decreased muscle mass, and mood disturbances.
Hypergonadism: Conversely, high testosterone levels, known as hypergonadism, may be indicative of conditions such as polycystic ovary syndrome (PCOS) in women or androgen-secreting tumors in men and women. Symptoms may include acne, hirsutism (excessive hair growth), menstrual irregularities, and masculinisation in women.
Infertility: Testosterone levels play a critical role in sperm production and male fertility. Abnormal total testosterone levels may contribute to male infertility, either through impaired spermatogenesis or disruptions in reproductive hormone balance.
Erectile Dysfunction (ED): Testosterone deficiency is associated with an increased risk of erectile dysfunction, which can affect sexual performance and intimacy. Low testosterone levels may contribute to ED by affecting libido, arousal, and the physiological processes involved in achieving and maintaining an erection.
Osteoporosis: Testosterone plays a role in maintaining bone density and strength, particularly in men. Low testosterone levels have been linked to an increased risk of osteoporosis and bone fractures, as testosterone deficiency can lead to decreased bone mineral density and increased bone resorption.
Metabolic Syndrome: Testosterone levels are inversely associated with metabolic risk factors such as obesity, insulin resistance, dyslipidemia, and hypertension. Low testosterone levels can contribute to the development of metabolic syndrome, i.e., conditions that increase the risk of cardiovascular disease and type 2 diabetes.
Cardiovascular Disease : Low testosterone levels have been linked to an increased risk of cardiovascular disease, including coronary artery disease, heart failure, and stroke. Testosterone deficiency may adversely affect lipid metabolism, vascular function, and inflammation, contributing to cardiovascular risk.
Mood Disorders: Testosterone influences mood regulation, and low testosterone levels have been associated with an increased risk of depression, anxiety, and mood disturbances in both men and women.
Muscle Weakness and Fatigue: Testosterone plays a role in maintaining muscle mass, strength, and energy levels. Low testosterone levels may result in muscle weakness, fatigue, and decreased physical performance.
In conclusion, the testosterone total test serves as a valuable diagnostic tool for identifying various health conditions related to testosterone levels in the body. By measuring the total amount of testosterone present in the blood, this test can aid in the detection of conditions such as hypogonadism, infertility, erectile dysfunction, and certain types of cancer. Additionally, abnormalities in testosterone levels may provide insights into underlying metabolic disorders, cardiovascular risks, and bone health issues. Overall, the testosterone total test plays a crucial role in assessing and managing a wide range of health conditions, ultimately contributing to the overall well-being and health of individuals. Book a Testosterone Total Test in Sasara for ONLY ₹670*
Who Should Get Tested?
How Does A Testosterone Total Test Work?
Blood Sample Collection: The test begins with the collection of a blood sample from the patient. A healthcare professional will perform a venipuncture, inserting a needle into a vein, usually in the arm, to draw a blood sample. The blood is then collected into a special tube or vial for analysis.
Laboratory Analysis:
Sample Processing: In the lab, the blood sample undergoes processing to separate the serum or plasma, which contains the analyte of interest—testosterone—from other blood components such as red blood cells.
Testosterone Measurement: Testosterone levels in the serum or plasma are measured using validated assays. This may involve techniques such as immunoassays or liquid chromatography-mass spectrometry (LC-MS), which detect and quantify testosterone based on specific interactions or molecular properties.
Calibration and Quality Control: Calibration standards and quality control samples are included in the analysis to ensure accuracy and reliability. Calibration standards establish the relationship between the measured signal and testosterone concentration, while quality control samples assess assay performance.
Result Reporting: Once the analysis is complete, the laboratory generates a report detailing the patient's total testosterone levels. Testosterone levels are typically expressed in units such as nanograms per deciliter (ng/dL) or picograms per milliliter (pg/mL). The report may include reference ranges corresponding to different age groups and sexes to aid in result interpretation.
Interpretation by Healthcare Provider: The test results are interpreted by the patient's healthcare provider in conjunction with their medical history, symptoms, and relevant clinical information. Deviations from normal testosterone levels may indicate hormonal imbalances or underlying health conditions, prompting further evaluation and management as necessary.
How To Prepare For A Testosterone Total Test?
Consult with Your Healthcare Provider: Before the test, discuss any medications or supplements you're taking with your healthcare provider. Some medications can affect testosterone levels, so your provider may advise adjusting or temporarily discontinuing them before the test.
Follow Fasting Instructions: Depending on your healthcare provider's instructions, you may need to fast for a certain period before the test. Typically, fasting for 8 to 12 hours overnight is recommended. However, if fasting is not required, you can eat and drink as usual before the test.
Avoid Strenuous Exercise : Refrain from engaging in vigorous physical activity or intense exercise for at least 24 hours before the test. Exercise can temporarily elevate testosterone levels, potentially affecting the accuracy of the results.
Stay Hydrated : Drink plenty of water in the days leading up to the test to ensure proper hydration. Being well-hydrated can facilitate blood sample collection and help maintain normal blood viscosity.
Follow Additional Instructions : Your healthcare provider may provide specific instructions tailored to your individual circumstances. Be sure to follow any additional guidance provided, such as abstaining from alcohol or caffeine before the test.
What Does The Test Results Mean?
The normal range for total testosterone levels can vary slightly between laboratories and is influenced by factors such as age, sex, and the specific assay method used for testing. However, as a general guideline, the typical reference range for total testosterone in adult males is approximately 300 to 1,000 nanograms per deciliter (ng/dL) or 10.41 to 34.67 nanomoles per liter (nmol/L). In females, the normal testosterone range typically falls between 8 to 60 nanograms per deciliter (ng/dL) in adults, with variations depending on factors such as age and individual health conditions. It's important to note that testosterone levels in females can fluctuate throughout the menstrual cycle and can be affected by factors such as pregnancy, menopause, and certain medical conditions. Therefore, testosterone levels should be interpreted in the context of an individual's overall health and symptoms.
Testosterone Range in Healthy Males
| Over Age 60 | |
|---|---|
| Total Testosterone | 600-800 ng/dL |
| Free Testosterone | 150-250 pg/mL |
| DHT | 30-60 ng/dL |
| Estradiol | 30-60 pg/mL |
| Under Age 60 | |
|---|---|
| Total Testosterone | 800-1100 ng/dL |
| Free Testosterone | 250-450 pg/mL |
| DHT | 30-60 ng/dL |
| Estradiol | 30-60 pg/mL |
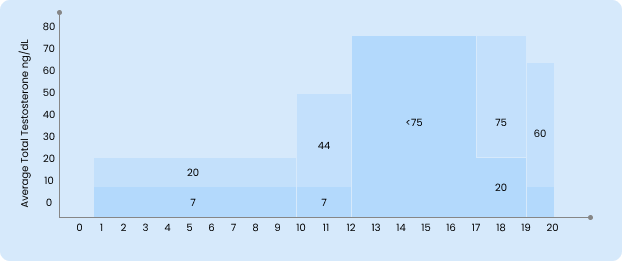
Average Testosterone By Age For Women
Risks Associated With A Testosterone Total Test
Discomfort or Pain: Some individuals may experience mild discomfort or pain at the site of the blood draw during venipuncture. This sensation is typically temporary and resolves quickly after the procedure.
Bruising or Hematoma: Bruising or hematoma (a localised collection of blood outside the blood vessels) may occur at the puncture site following the blood draw. This is more common in individuals with fragile or easily bruised skin and usually resolves within a few days.
Infection: While rare, there is a minimal risk of infection at the puncture site. Healthcare providers follow strict sterile procedures to minimise this risk, including disinfecting the skin before the blood draw and using sterile equipment.
Fainting or Lightheadedness: Some individuals may experience fainting, lightheadedness, or dizziness during or after the blood draw, particularly if they have a fear of needles or are prone to vasovagal reactions. Healthcare providers take precautions to ensure patient comfort during the procedure.
Rare Complications: In extremely rare cases, more serious complications such as nerve damage or arterial puncture may occur. However, these complications are exceedingly uncommon and typically occur due to improper technique or underlying anatomical abnormalities.
In conclusion, the testosterone total test is a generally safe and minimally invasive diagnostic procedure with few associated risks. The procedure involves a simple blood draw, which carries minimal discomfort and typically no serious complications. While rare, potential risks such as bruising, fainting, or infection at the site of the blood draw may occur. However, these risks are generally minor and easily managed. Overall, the benefits of obtaining valuable diagnostic information regarding testosterone levels often outweigh the minimal risks associated with the test. As with medical procedures, it's essential for healthcare providers to inform patients about potential risks and ensure proper precautions are taken to mitigate them. Book a Testosterone Total Test in Sasara for ONLY ₹670*
Holistic Approaches To Maintain Good Testosterone Levels In Your Body
Healthy Diet:Engaging in regular physical activity, including both cardiovascular exercise and strength training, can help maintain healthy testosterone levels. Aim for a combination of aerobic exercises (running, cycling) and resistance training (weightlifting, bodyweight exercises) to optimise hormonal balance and fitness.
Regular Exercise:Engaging in regular physical activity, including both cardiovascular exercise and strength training, can help maintain healthy testosterone levels. Aim for a combination of aerobic exercises (running, cycling) and resistance training (weightlifting, bodyweight exercises) to optimise hormonal balance and fitness.
Manage Stress:Chronic stress can negatively impact hormone levels, including testosterone. Incorporate stress-reduction techniques such as mindfulness meditation, deep breathing exercises, yoga, tai chi, or spending time in nature to help manage stress levels and support hormonal balance.
Adequate Sleep:Prioritise getting sufficient sleep each night, as inadequate sleep can disrupt hormone production and regulation, including testosterone. Aim for 7-9 hours of quality sleep per night to support overall health and hormone balance.
Maintain Healthy Body Weight:Obesity and excess body fat can contribute to hormonal imbalances, including lower testosterone levels. Maintaining a healthy body weight through a combination of diet, exercise, and lifestyle modifications can help support hormonal balance.
Limit Alcohol and Avoid Substance Abuse:Excessive alcohol consumption and substance abuse can negatively impact testosterone levels and overall health. Limit alcohol intake and avoid illicit drug use to support hormone balance and overall well-being.
Herbal Supplements:Some herbal supplements may have potential benefits for supporting testosterone levels, although research results are mixed. Examples include ashwagandha, Tribulus terrestris, fenugreek, and Tongkat Ali. However, it's essential to consult with a healthcare provider before using herbal supplements, as they may interact with medications or have contraindications.
Avoid Environmental Toxins:Minimise exposure to environmental toxins and endocrine-disrupting chemicals found in plastics, pesticides, and personal care products. Choose natural and organic alternatives to reduce toxin exposure and support hormone balance.